Weighing the future of healthcare
OZEMPIC'S BENEFITS GO BEYOND WEIGHT LOSS. AUSTRALIA'S HEALTH POLICY MUST CATCH UP.

Weight loss drugs like Ozempic and Mounjaro are making headlines for its dramatic impact on weight loss, but the true potential of these drugs go far beyond the scale. Yet access remains limited. GP and Assistant Professor of General Practice Dr Kieran Le Plastier explains why we should quit moralising and embrace the potential of these drugs to reshape the future of public health.
It’s rare in medicine to witness a single class of drugs redefine the boundaries of treatment across multiple chronic diseases. Yet that’s precisely what we’re seeing with GLP-1 receptor agonists — commonly known by brand names including Ozempic and Mounjaro.
Initially developed as a treatment for diabetes, these drugs are now proving to be nothing short of transformative for millions of people worldwide. But while their potential is vast, our access to them remains frustratingly narrow.
The expanding potential of GLP-1s
There’s a common misconception that these drugs are only a tool for weight loss and diabetes management. But that’s far from the limit of their potential.
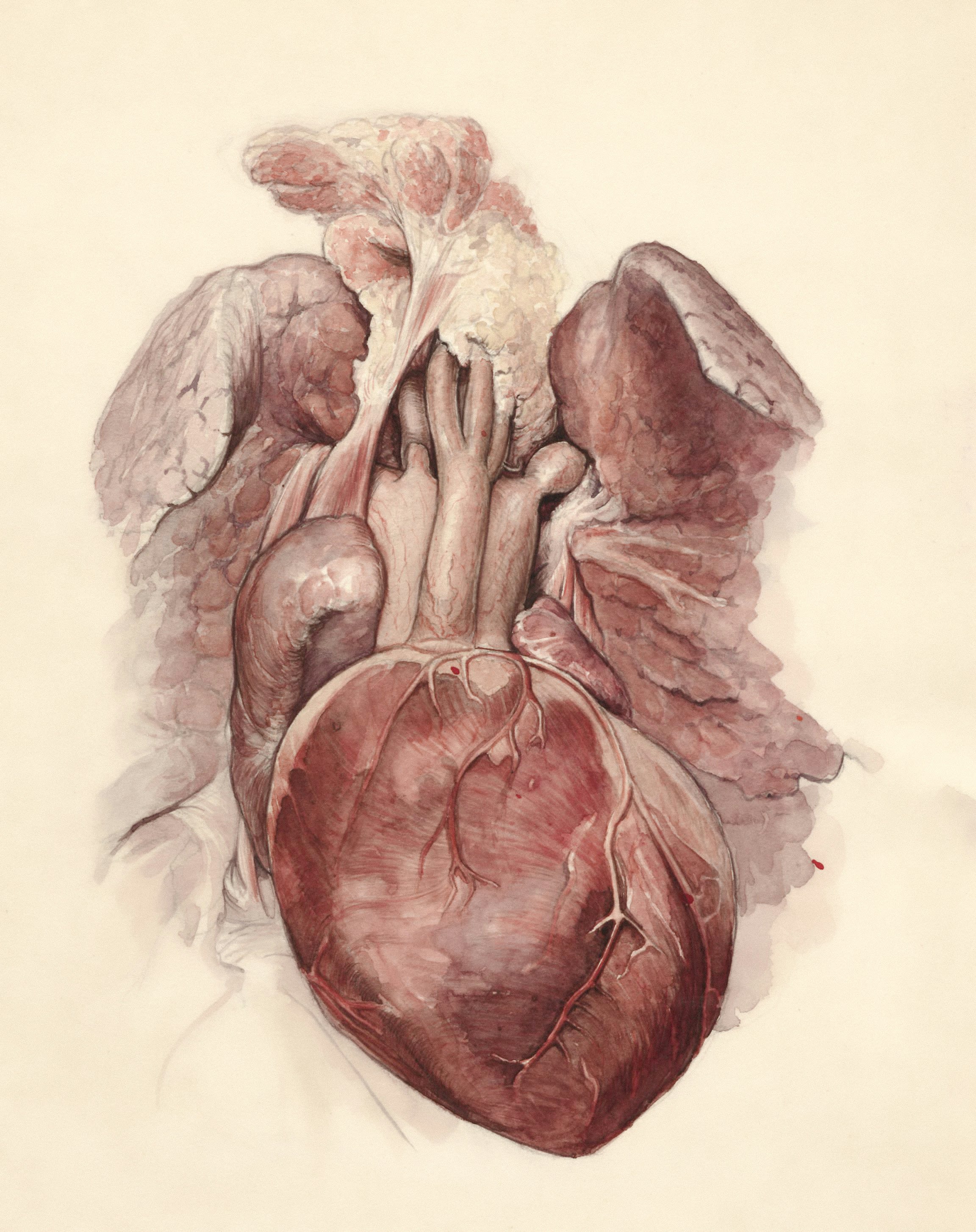
These medications are showing promise in reducing the risk of heart disease, stroke, kidney failure, liver disease, and even dementia.
They’re also being explored as tools to combat addiction — blunting the brain’s reward system and helping people overcome dependencies on alcohol, nicotine, and other substances.
The access gap
We are standing at the edge of a paradigm shift in how we treat chronic disease.
Yet in Australia, access to these drugs is largely restricted to people with uncontrolled diabetes at a subsidised cost under the Pharmaceutical Benefits Scheme.
While they can be prescribed off-label for other conditions, such as obesity, without the PBS subsidy the cost can be anything from $55 to $130 a dose, which most people simply can’t afford.
Obesity is not a personal moral failing. It is a complex, multi-factorial condition driven by genetics, environment, and a society that promotes sedentary lifestyles and calorie-dense foods.
We live in an obesogenic world, and blaming individuals for their biology is both unjust and ineffective.
Global momentum
The UK’s NHS has already recognised this, moving to subsidise GLP-1 drugs for people with obesity to reduce long-term disease burden.
Australia must follow suit. The cost of inaction — measured in heart attacks, strokes, hospital admissions, and lives lost — is far greater than the cost of these medications.
Now, these drugs are not a silver bullet. They work best as part of a holistic approach that includes dietary support, physical activity, and psychological care.
And as for every powerful therapeutic drug, risks exist and must be carefully considered and managed under the care of expert health practitioner
But they offer something we’ve never had before: a safer, effective, and scalable way to intervene in the metabolic cascade that underpins so many of our modern diseases.
We need to stop treating these drugs as luxury items for the wealthy or as quick fixes for vanity.
They are powerful tools for prevention and healing.
It’s time our health system caught up with the science.
Published Wednesday, 27 August, 2025.
Original thinking direct to your inbox

Stories from Bond
