Sugar, how sweet it is. But could it be causing you gastrointestinal distress? Senior Teaching Fellow and nutrition scientist Dr Carolyn English explains how a sugar intolerance may be behind a common gastrointestinal issue.
Ever feel bloated? Have excess gas? Running to the loo too many times? Many people experience these digestive issues, which may actually be a sign that they are unable to digest certain sugars — like sucrose.
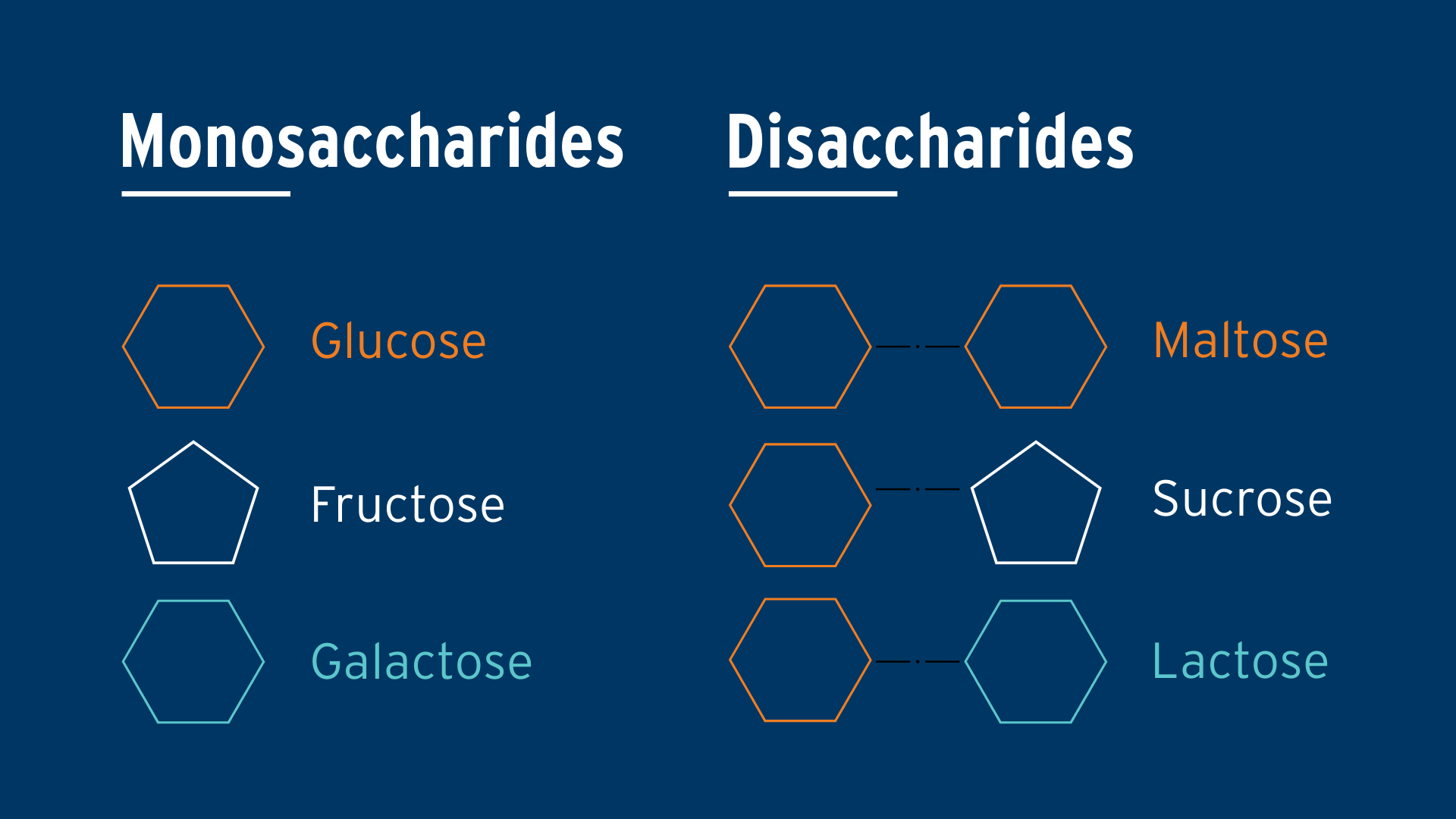
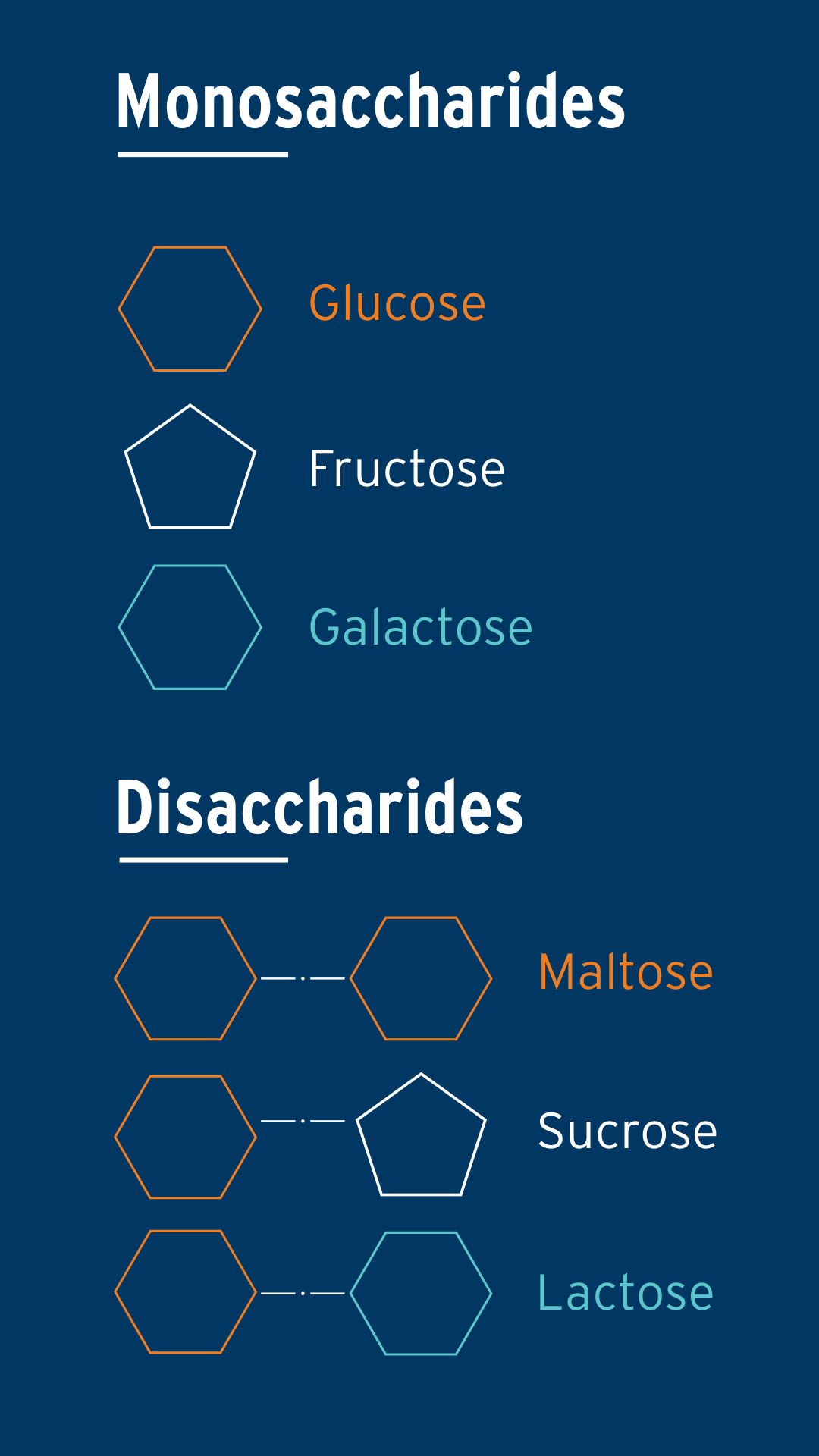
Sugars are carbohydrates and come in two main types: single sugars (monosaccharides) like glucose and fructose, and double sugars (disaccharides). Double sugars must be broken down into single sugars by enzymes, as the body can only absorb them once they're in their simplest form. Table sugar, or sucrose, is a double sugar made of glucose and fructose bonded together. To digest sucrose, our intestines use the enzyme sucrase-isomaltase to break the bond between glucose and fructose, allowing the individual sugars to be absorbed. Sucrase-isomaltase also breaks down some maltose, a sugar from starch in foods like bread, pasta, rice, and potatoes.


However, if your body doesn’t produce enough of this enzyme, the sucrose is unable to be broken down and absorbed. As a result, sucrose travels to the colon where gut bacteria ferment it, producing excess gas, abdominal cramping and bloating. This process can also draw excessive water into the area, leading to diarrhoea. In some individuals, sucrose intolerance can even cause constipation or reflux.
This process is similar to lactose intolerance, where some individuals lack the enzyme lactase, which breaks the bond between glucose and galactose, (the two simple sugars bound together to make lactose, found in dairy products). Lactose intolerance affects about 70 per cent of the adult world population and can lead to symptoms like gas, bloating, and diarrhoea after drinking milk.
Until recently, it was believed that sucrose intolerance was only found in the rare genetic disorder known as Congenital sucrase-isomaltase deficiency (CSID). In individuals with CSID, the enzyme is either deficient or absent, preventing the digestion of sucrose and maltose, which leads to gastrointestinal symptoms. CSID is typically diagnosed in infants who struggle to thrive due to an inability to absorb sucrose and starch properly.
However, a recent study found that 35 per cent of people who underwent biopsies during endoscopies for IBS had low sucrase-isomaltase activity. This suggests that this enzyme deficiency is more common than previously thought and may be a contributing factor in IBS symptoms.
In addition to CSID, new evidence has revealed another condition called Acquired sucrase-isomaltase deficiency (ASID), which is characterised by low levels of the sucrase-isomaltase enzyme. This condition can be transient and may result from damage to the lining of the gut due to infection or inflammation. Additionally, research has uncovered a common genetic mutation in the sucrase-isomaltase gene (known as 15PHE). This mutation results in a 35 per cent reduction in the enzyme's activity, which can lead to digestive symptoms similar to IBS. Even carrying one copy of the 15PHE gene increases the risk of IBS.
In today’s food environment where sugar is added to everything from tomato sauce to peanut butter, this may be causing distress for many people.
You have probably heard of a low FODMAP diet. It is widely considered the most effective dietary treatment for IBS. FODMAPs are short-chain carbohydrates or sugars that the small intestine can't absorb. They travel to the large intestine, where gut bacteria ferment them. However, for some people — particularly those with IBS — this fermentation process produces a lot of gas and digestive discomfort. While the low FODMAP diet helps many IBS patients, up to 50 per cent do not see significant symptom relief.

Could it be that some people need to eliminate a different type of sugar from their diet?
Several randomised clinical trials led by researchers at Lund University and Skåne University Hospital in Sweden tested a low-sucrose, low-starch diet for patients with IBS. These studies found that this diet significantly reduced abdominal pain, bloating, and diarrhoea and improved extra-intestinal symptoms, such as muscle, joint pain, and fatigue.
A recent follow-up study compared this low-sucrose, low-starch diet to the low FODMAP diet to evaluate which one was more effective. Both diets showed similar improvements in gastrointestinal and extra-intestinal symptoms. However, the low-sucrose, low-starch diet led to greater reductions in weight and sugar cravings compared to the low FODMAP diet, and was preferred by participants who found it easier to adhere to.
What did the low-sucrose, low-starch diet entail? All sources of sucrose were removed, and starch was limited to two servings a day - either ½ cup of oats or one slice of whole grain bread, and either ½ a cup of brown rice or whole grain pasta. Participants were also advised to avoid specific fruits and vegetables high in sucrose such as mangoes, apples, oranges, carrots, corn and beetroot. Instead, they were encouraged to consume lower-sucrose varieties like berries, grapes, pears, leafy greens, green beans, and broccoli. All other foods, including dairy, eggs, poultry, and meats, were allowed, as well as sweeteners that don’t contain sucrose (like honey and agave syrup).
How do I know if I am malabsorbing sucrose?
To diagnose sucrose intolerance you need to see your GP or dietitian, who may order a breath test. However, the gold standard for diagnosis is a biopsy of your intestine to check your enzyme activity, which is done under anesthesia by a gastroenterologist.
However, there is a simple at-home test that has been shown in a small study to help identify sucrose intolerance. This is called the “4-4-4 Test.” In the morning, while fasted, drink a solution of 4 tablespoons of table sugar (about 60 grams) mixed with 4 ounces of water (120 millilitres) and wait 4 hours. If you experience digestive issues such as bloating, diarrhea, or gas during this time, it may indicate that you're malabsorbing sugar.
Alternatively, you can try limiting sucrose and eating less starch to see if you feel better. Regardless of whether you have sucrose intolerance, reducing your sugar intake may improve your digestion and overall well-being, helping you feel better.
Published on Wednesday, 21 May, 2025.
Original thinking direct to your inbox

Stories from Bond